Pelvic floor exercise , often known as Kegel exercises, helps to relax and develop these muscles, which improves blood flow and eases tense muscles. These exercises, which were first designed to treat urine incontinence, now physical therapy for vulvodynia have demonstrated encouraging outcomes in the treatment of vulvar pain and discomfort.
Vulvodynia is a persistent form of pain or discomfort in the area surrounding the vulva, outer portion of the female reproductive organ. Vulvodynia-related pain, burning, or irritation can be so unbearable that it becomes impossible to sit still or engage in sexual activity.
Irritation or hypersensitivity of the nerve fibers in the vulval skin may cause this disorder. Due to abnormal nerve fibers, pain is perceived without physical contact
The first stage of physical therapy for vulvodynia is to learn how to relax the pelvic floor. Several treatments can help desensitize the vulval area.
Which symptoms of vulvodynia are present?
The primary sign of vulvodynia is pain in the vulva, which involves vaginal opening.
- Burning is common in valvular pain.
- Burning.
- Discomfort.
- Irritating.
- Muscle soreness.
- A sensation of sharp, knife-like pain.
Dyspareunia, or pain during sexual activity, can be brought on by vulvodynia, which can also affect your ability to sit, stand, and even sleep soundly. Vulvodynia is a medical disorder that causes chronic pain and is treatable.
Vulvodynia pain can hurt your overall health, physical comfort, and relationships. Many women use vaginal dilators to treat vulvodynia, and there is no doubt that they can be very effective. Chronic discomfort does not have to be a way of life, although overcoming vulvodynia symptoms can be time-consuming and difficult. There are some pelvic floor exercises for vulvodynia other than dilators that will help you relieve valvular pain.
What are the causes of vulvodynia?
Possible causes of vulvodynia include:
- vulval nerve injury, nerve irritation or over-sensitivity.
- , prior vaginal infections.
- hormonal fluctuations (e.g. estrogen),
- weak pelvic floor muscles. Muscular spasms.
- Inflammation.
- Genetic (inherited) factors.
- Nerve injury (neuropathy).
- Previous vaginal infections can cause long-term effects.
- Weak pelvic floor muscles or
- Harsh products can irritate your skin.
Research suggests that Vulvar pain affects up to 20% of women at some time in their lives, and the majority of those who experience it have pelvic floor problems. Pelvic floor dysfunction in women is associated with considerable functional restrictions due to painful intercourse, urine, bowel, and sexual dysfunction. A fast pelvic floor muscle screening can be conducted in the gynecology office and should be used when patients report pelvic pain complaints.
How to diagnose vulvodynia?
The diagnosis is based on medical history and a pelvic examination.
- Pelvic examination: A doctor might take a sample of cells from the vagina to test for an infection caused by yeast or bacteria.
- Cotton swab test: A moistened cotton swab is gently used to examine for specific pain regions in your vulva.
- Biopsy: If the skin of the vulva appears different than usual, your doctor or gynecologist may extract a small tissue sample for testing at a laboratory.
What are the treatment options available for vulvodynia?
- Antidepressants and anticonvulsants: These can help relieve chronic discomfort. Some antidepressants come in creams that can be applied to the skin.
- Local anesthetics. These medications can provide temporary pain relief. For example, you may apply lidocaine ointment to your vulva 30 minutes before sex to make it more comfortable.
- Nerve blocks. These injections are administered near a pain-sensitive nerve or group of nerves. These may be useful if chronic pain does not respond to other therapies.
- Hormonal creams. If hormonal changes cause your problems, vaginal estrogen cream may provide relief. Sometimes, hormonal cream may be used in conjunction with testosterone cream.
- Antihistamines. These medications, commonly used to treat allergies, may also help alleviate vulvodynia symptoms. However, antihistamines may be irritating if you have passed menopause.
How do pelvic floor exercises for vulvodynia help treat it?
- Pelvic floor therapy. Pelvic floor exercise for vulvodynia stretches and relaxes such muscles and can help to alleviate vulvodynia pain.
- Kegel exercise: To relax the muscles around your vagina, start incorporating Kegel exercises into your regular schedule. If you can insert objects into your vagina, vaginal cones are utilized to improve your Kegel exercises and eventually desensitize the area to pressure.Your physical therapist may also prescribe that you use a home vaginal dilator, which stretches and stimulates the vagina.
- Abdominal breathing: Abdominal breathing is a relaxing technique in which the individual concentrates on taking calm, deep breaths. It involves slowly breathing in through the nose and then out through the mouth with the diaphragm.
- Biofeedback: Biofeedback and Kegel (pelvic floor) exercises. An electrical biofeedback gadget can be used to score the strength of your muscles while you squeeze against a vaginal probe, allowing you to learn how to execute more effective Kegels and track your progress.
- Transcutaneous electrical nerve stimulation : It (TENS) is commonly used to alleviate pain during labor, persistent back pain, and other chronic pain problems. It works by inhibiting the pain signal transmitted to the brain, which can be beneficial for some women experiencing vulval pain. TENS should be used once or twice weekly for 6–8 weeks.
- The nerve-stimulating apparatus can be applied to the lower back, where the nerves supplying the vulvular area exit the lower spine or through a probe inserted into the vagina.
- Trigger point release: Vulvar pain can cause trigger points in the pelvic floor muscles, which are sites of tightness or tension. It would help you to determine whether you have such trigger points and learn proper strategies to relieve the tightness. These procedures are comparable to those utilized by physiotherapists, who treat low back discomfort and joint or muscle injuries.
What Lifestyle modification should be modified to treat vulvodynia symptoms?
Simple self-care techniques may assist you in managing vulvodynia symptoms.
- Get comfortable. If you often sit during the day, utilize a foam rubber doughnut cushion.
- Try to stand more. It relieves pressure on the areas surrounding your vulva.
- Limit high-intensity exercises like running. These generate friction, which can irritate the vulva.
- Following exercise, use a frozen gel pack. Wrap it in a towel and place it on your vulva for up to 15 minutes to alleviate symptoms.
- Limit activities that create pressure on your vulva, such as cycling or horseback riding.
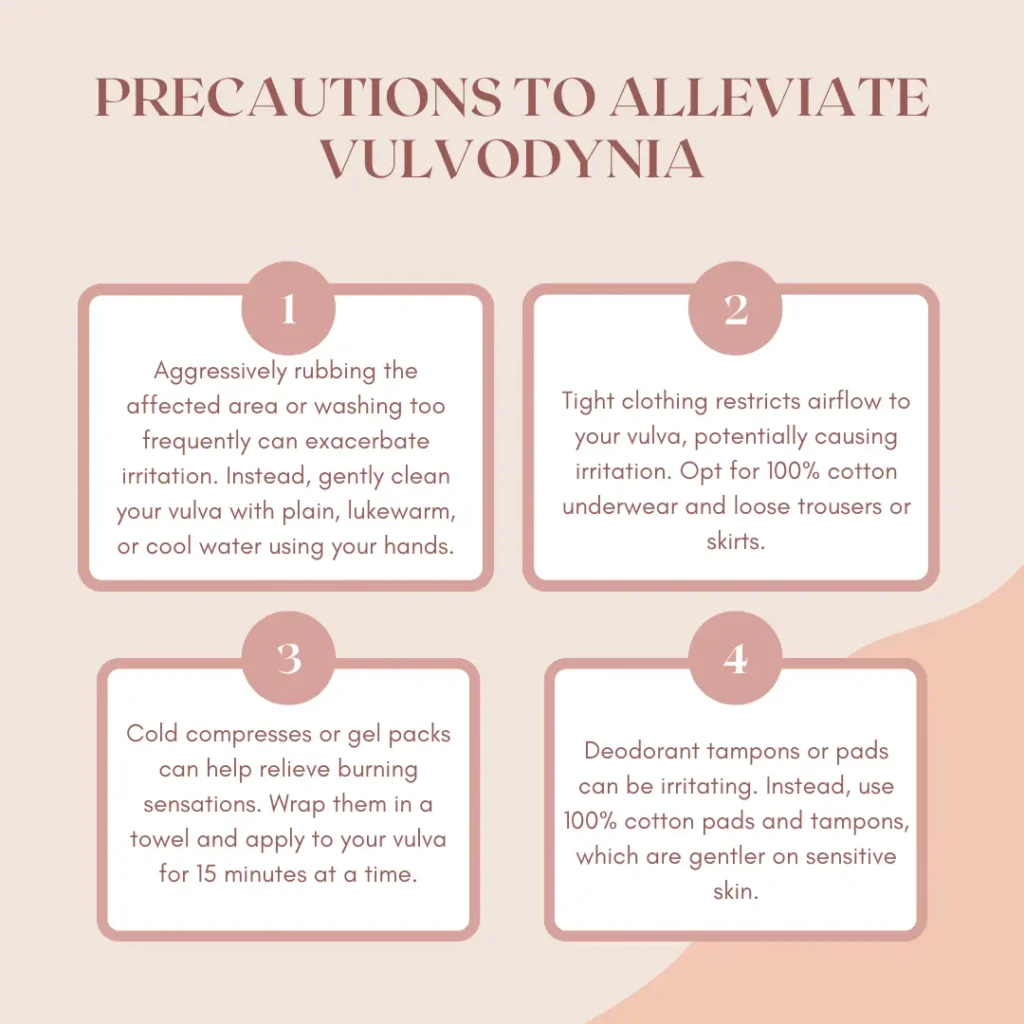
What are the precautions one should take to alleviate vulvodynia?
Bathing and swimming tips include the following:
- Wash it carefully. Aggressively rubbing the affected region or washing too frequently can aggravate irritation. Instead, gently wipe your vulva with plain, lukewarm, or cool water in your hands. Then, pat dry the area. After your bath, apply a preservative-free lubricant, such as basic petroleum jelly, to form a protective barrier.
- Avoid products that could irritate the vulva. Avoid using bubble baths, feminine hygiene products, fragrant creams, or soap.
- Swim in pools without a lot of chlorination. These pools disinfectant and keep the water clean, but too much might irritate it.
- Soak in a sits bath. Sit for 5 to 10 minutes in lukewarm or chilly water containing Epsom salt two to three times daily. This may help alleviate burning and irritation.
- Stay out of hot pools and baths. Spending time in hot water can be uncomfortable and itchy.
- Some hygiene advice includes not using deodorant tampons or pads. Deodorant can be annoying. Instead, use 100% cotton pads and tampons.
- Use soft, white, unscented toilet paper.
- Urinate before your bladder becomes full. Then, clean your vulva with water and pat dry.
Here are some tips regarding clothing and laundry:
- Wear loose-fitting clothing. Tight clothing restricts airflow to your vulva, potentially irritating the area. Wear 100% cotton pants. Also, wear loose trousers and skirts. Remove your exercise clothes as soon as you finish your workout. It would help if you also took off your swimming suit after you swim.
- If your washing machine offers a double- or extra-rinse cycle, use it for garments that come into contact with your vulva. It aids in the rinse-off process.
If you are sexually active,
- Use water-based lubricant and Put it on before having sex. Avoid using goods that contain alcohol, colors, perfume, flavor, or warming or cooling agents.
- Choose your birth control with caution. Keep in mind that spermicide or contraceptive creams may irritate. Consult your doctor or another member of your care team about a method of birth control that will not irritate your vulva.
- Urinate after sex. It helps to reduce your risk of getting an infection. After urinating, clean your vulva with cool water and pat it dry.
- Cold compresses or gel packs can help relieve burns. Wrap them in a towel and apply them to your vulva for 15 minutes at a time.



